Kicking off with the very best antibiotic for blended urogenital flora infections, this opening paragraph is designed to captivate and have interaction the readers, setting the tone for an informative dialogue in regards to the pressing care and therapy choices obtainable for this situation.
Blended urogenital flora infections could cause a spread of signs, from delicate discomfort to extreme problems, so it is important to deal with the problem promptly and successfully. On this article, we’ll discover the very best antibiotics for blended urogenital flora infections, factoring in elements reminiscent of affected person allergic reactions, an infection severity, and native antibiotic resistance patterns.
Pressing Look after Blended Urogenital Flora
Blended urogenital flora infections can result in a spread of problems if left untreated or undertreated. These problems might embody pelvic inflammatory illness (PID), infertility points, and an elevated danger of sexually transmitted infections (STIs).
Understanding the urgency of treating blended urogenital flora infections is important in stopping long-term harm. Delayed intervention can result in extreme penalties, making immediate therapy important.
Widespread Signs and Problems
Blended urogenital flora infections can exhibit a wide range of signs, usually overlapping with these of different situations. Recognizing these signs early is essential for acquiring immediate medical consideration.
* Widespread signs:
* Dysuria (painful urination)
* Elevated frequency of urination
* Urinary urgency
* Pelvic ache or discomfort
* Irregular vaginal discharge
* Itching or burning sensation within the genital space
* Problems:
-
* Pelvic inflammatory illness (PID)
* Infertility or reproductive points
* Elevated danger of sexually transmitted infections (STIs)
* Persistent pelvic ache
* Urinary tract infections (UTIs)
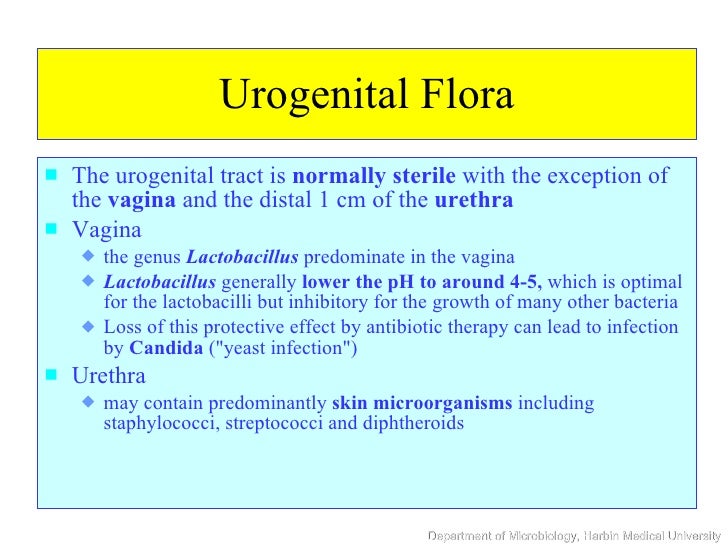
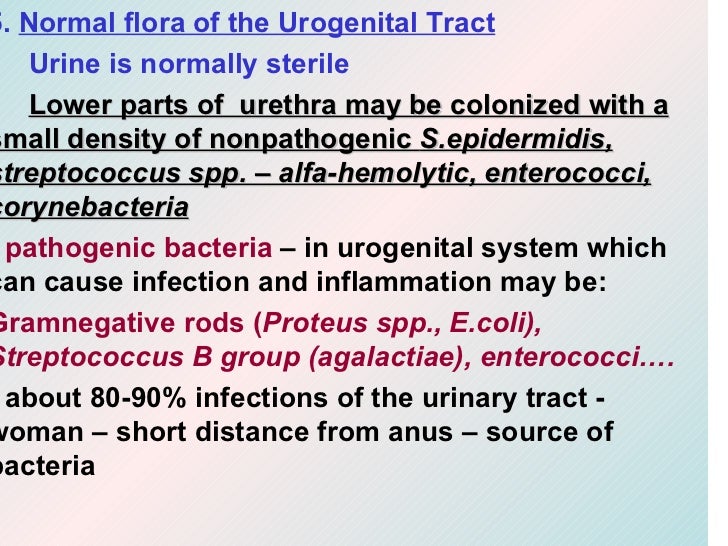
Bacterial Causative Brokers of Urogenital Tract Infections
Understanding the micro organism chargeable for urogenital tract infections is essential in deciding on efficient antibiotics. Widespread bacterial pathogens embody.
-
* Escherichia coli (E. coli)
* Staphylococcus saprophyticus
* Streptococcus agalactiae (Group B strep)
* Gardnerella vaginalis
* Atopobium vaginae
Pressing Care and Remedy Choices
Immediate intervention is essential in managing blended urogenital flora infections. Remedy sometimes entails antibiotics, though particular choices might range relying on the causative agent, severity of signs, and particular person affected person elements.
Applicable therapy must be initiated promptly to stop long-term harm and problems.
Antibiotic Choice and Utilization
Choosing the best antibiotic for blended urogenital flora infections is essential. When deciding on antibiotics, take into account the next elements:
-
* Causative agent: Antibiotic choice must be guided by the suspected or confirmed bacterial pathogens.
* Severity of signs: Extra extreme signs might require broad-spectrum antibiotics.
* Affected person’s medical historical past: Pregnant or breastfeeding ladies, people with kidney or liver illness, and people allergic to sure antibiotics require particular consideration.
* Resistance patterns: Native resistance patterns must be thought of when deciding on antibiotics.
* Remedy length: Brief-course vs. extended therapy regimens must be fastidiously evaluated.
Antibiotic Choices for Blended Urogenital Flora: Greatest Antibiotic For Blended Urogenital Flora

Blended urogenital flora infections, which will be attributable to a mix of pathogens reminiscent of Escherichia coli, Staphylococcus saprophyticus, Klebsiella pneumoniae, and others, require the collection of an efficient antibiotic for therapy. On this context, selecting the best antibiotic is essential to make sure the eradication of the an infection and decrease the event of antibiotic resistance.
One of many important elements in deciding on an antibiotic for blended urogenital flora is its efficacy in opposition to a broad spectrum of pathogens. As well as, the security profile of the antibiotic, together with its potential uncomfortable side effects and interactions with different medicines, is essential.
The mechanisms of motion for generally used antibiotics embody inhibiting bacterial cell wall synthesis (betalactams), disrupting DNA synthesis (quinolones), and inhibiting the motion of important bacterial enzymes (sulfa medication).
Betalactam Antibiotics
Betalactam antibiotics, together with penicillins and cephalosporins, work by inhibiting the synthesis of the bacterial cell wall. This results in the weakening of the cell wall, inflicting the bacterial cell to die.
- Amoxicillin: Amoxicillin is a beta-lactam antibiotic generally used to deal with a spread of bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting the synthesis of the bacterial cell wall.
- Ceftriaxone: Ceftriaxone is a cephalosporin antibiotic that’s used to deal with bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting the synthesis of the bacterial cell wall.
Quinolone Antibiotics
Quinolone antibiotics work by inhibiting DNA gyrase, an enzyme important for bacterial DNA replication. This results in the inhibition of bacterial progress and replication.
- Ciprofloxacin: Ciprofloxacin is a quinolone antibiotic generally used to deal with a spread of bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting DNA gyrase.
- Levofloxacin: Levofloxacin is a quinolone antibiotic used to deal with bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting DNA gyrase.
Sulfa Medicine
Sulfa medication work by inhibiting folic acid synthesis in bacterial cells. This results in the inhibition of bacterial progress and replication.
- Sulfamethoxazole: Sulfamethoxazole is a sulfa drug generally used to deal with a spread of bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting folic acid synthesis.
- Trimethoprim: Trimethoprim is a sulfa drug used to deal with bacterial infections, together with blended urogenital flora. It’s a broad-spectrum antibiotic that works by inhibiting folic acid synthesis.
Elements Influencing Antibiotic Alternative for Blended Urogenital Flora
Affected person-related elements play a pivotal position in figuring out the selection of antibiotic for treating blended urogenital flora infections. These elements not solely affect the effectiveness of the therapy but additionally decrease the chance of opposed reactions and optimize affected person outcomes.
Affected person-Associated Elements
Affected person-related elements that influence antibiotic selection embody allergic reactions, being pregnant, and lactation. A radical medical historical past of the affected person is essential in deciding on an acceptable antibiotic.
• Allergic reactions: Sufferers with recognized allergic reactions to sure antibiotics must be excluded from therapy with these specific antibiotics.
• Being pregnant and Lactation: Antibiotics must be chosen with warning in pregnant and lactating ladies, as some could also be teratogenic or excreted in breast milk.
An infection Severity and Period
The severity and length of the an infection additionally play a vital position in figuring out the kind of antibiotic for use. In instances of extreme or extended an infection, broad-spectrum antibiotics could also be crucial to make sure efficient therapy.
• Severity of An infection: Extreme infections might require broad-spectrum antibiotics to cowl a variety of pathogens.
• Period of An infection: Extended infections might necessitate the usage of antibiotics with longer half-lives to take care of efficient concentrations over time.
Native Antibiotic Resistance Patterns
Native antibiotic resistance patterns are a important think about guiding therapy choices. The selection of antibiotic must be based mostly on the prevalence of resistant pathogens in the neighborhood.
Based on the Facilities for Illness Management and Prevention (CDC), antibiotic resistance is a rising concern globally, with many micro organism growing resistance to generally used antibiotics.
• Prevalence of Resistant Pathogens: Areas with excessive charges of antibiotic resistance might require the usage of various antibiotics or mixture remedy.
• Antimicrobial Stewardship: Healthcare suppliers ought to guarantee accountable antibiotic use by implementing antimicrobial stewardship applications to cut back the event of antibiotic resistance.
Desk of Native Antibiotic Resistance Patterns
| Antibiotic | Resistant Pathogens | Vulnerable Pathogens |
| — | — | — |
| Amoxicillin | Micro organism reminiscent of Escherichia coli (E. coli) and Klebsiella pneumoniae | Sure strains of Staphylococcus aureus |
| Ciprofloxacin | Pseudomonas aeruginosa | Most strains of E. coli |
By contemplating these elements, healthcare suppliers could make knowledgeable choices about antibiotic selection for treating blended urogenital flora infections, in the end enhancing affected person outcomes and lowering the chance of antibiotic resistance.
Antibiotic Resistance and Blended Urogenital Flora
The rising prevalence of antibiotic-resistant micro organism poses a big problem within the therapy of blended urogenital flora infections. Improper use of antibiotics, reminiscent of overuse or misuse, has contributed to the event and unfold of antibiotic resistance amongst microorganisms.
The World Well being Group (WHO) has warned that the rise of antibiotic resistance is likely one of the greatest threats to international well being, meals safety, and improvement. Within the context of blended urogenital flora infections, insufficient therapy and pointless antibiotic use can have extreme penalties, together with extended sickness, elevated healthcare prices, and the transmission of resistant micro organism to others.
Methods for Lowering Antibiotic Resistance
A number of methods will be employed to cut back antibiotic resistance in blended urogenital flora infections:
- Applicable Use of Antibiotics:
- Antibiotic Stewardship:
- Various Remedy Approaches:
· Antibiotics must be prescribed solely when crucial, and for the shortest length required to deal with the an infection.
· The selection of antibiotic must be guided by native antibiograms and antibiotic susceptibility testing outcomes.
· Sufferers must be educated on the right use and potential uncomfortable side effects of antibiotics.
· Implementing antibiotic stewardship applications in healthcare settings can assist optimize antibiotic use and enhance affected person outcomes.
· These applications usually contain antibiotic committees, instructional initiatives, and audit and suggestions mechanisms.
· Non-antibiotic remedies, reminiscent of probiotics, prebiotics, and vaginal suppositories, could also be efficient in managing delicate instances of blended urogenital flora infections.
· Mixture remedy, the place a number of antibiotics are utilized in mixture, could also be useful in sure instances however requires cautious concerns.
· The usage of bacteriophage remedy, which entails the usage of bacteriophages (viruses that concentrate on particular micro organism), is being explored as a possible various therapy method.
Penalties of Insufficient Remedy and Pointless Antibiotic Use
The results of insufficient therapy and pointless antibiotic use will be extreme and far-reaching, together with:
- Extended Sickness:
- Elevated Healthcare Prices:
- Transmission of Resistant Micro organism:
· Untreated or inadequately handled infections can result in extended sickness and elevated morbidity.
· The event of antibiotic-resistant micro organism could make therapy tougher and extended.
· Insufficient therapy and pointless antibiotic use can lead to elevated healthcare prices because of the want for extended hospital stays, further testing, and various remedies.
· Resistant micro organism will be transmitted to others by person-to-person contact or contaminated meals and water.
· The unfold of resistant micro organism can have extreme penalties, together with the lack of efficient therapy choices and elevated mortality.
Monitoring Resistance and Rising Tendencies
Monitoring resistance and rising traits is important within the prevention and therapy of blended urogenital flora infections. This may be achieved by:
- Surveillance Packages:
- Antibiogram Growth:
- Rising Tendencies:
· Nationwide and worldwide surveillance applications can observe the prevalence and unfold of antibiotic-resistant micro organism.
· These applications usually contain the gathering and evaluation of knowledge on antibiotic-resistant infections.
· Antibiograms, which offer info on the susceptibility and resistance of microorganisms to numerous antibiotics, can be utilized to information therapy choices.
· Antibiograms must be up to date recurrently to mirror modifications in antibiotic resistance patterns.
· Rising traits, such because the rise of extensively drug-resistant (XDR) and pandrug-resistant (PDR) micro organism, will be monitored by surveillance applications and literature opinions.
Remedy Regimens and Administration Strategies
Remedy regimens for blended urogenital flora infections sometimes contain a mix of antibiotics and different medicines to deal with the assorted elements of the an infection. Efficient therapy regimens intention to eradicate the an infection whereas minimizing the chance of antibiotic resistance and uncomfortable side effects.
Widespread Dosage Kinds and Administration Strategies
There are a number of dosage types and administration strategies used to deal with blended urogenital flora infections, together with oral, intravenous, and topical medicines.
- Oral Medicines: Oral antibiotics are generally used to deal with blended urogenital flora infections. Examples embody fluoroquinolones (e.g., ciprofloxacin and levofloxacin), macrolides (e.g., azithromycin and clarithromycin), and penicillins (e.g., amoxicillin and ampicillin).
- Intravenous Medicines: Intravenous antibiotics could also be used for extra extreme infections or in hospitalized sufferers. For instance, cephalosporins (e.g., ceftriaxone and cefotaxime) and carbapenems (e.g., meropenem and imipenem) are generally used intravenous antibiotics for treating blended urogenital flora infections.
- Topical Medicines: Topical antibiotics could also be used for treating localized infections, reminiscent of vaginal or urinary tract infections. Examples embody metronidazole and clindamycin lotions or suppositories.
Efficient therapy regimens require cautious consideration of the affected person’s medical historical past, present well being standing, and the particular traits of the an infection. Sufferers ought to adhere to their therapy regimens as directed by their healthcare supplier to realize optimum outcomes and decrease the chance of uncomfortable side effects.
Significance of Adherence and Monitoring
Monitoring for uncomfortable side effects is essential throughout therapy. Healthcare suppliers ought to intently monitor sufferers for indicators of allergic reactions, gastrointestinal disturbances, and different potential uncomfortable side effects related to antibiotics. As well as, sufferers might expertise vaginal or urinary tract signs reminiscent of itching, burning, or discharge, which must be reported to their healthcare supplier.
Managing Antibiotic Resistance
To attenuate the chance of antibiotic resistance, sufferers ought to adhere to their therapy regimens as directed by their healthcare supplier. As well as, healthcare suppliers ought to comply with tips for acceptable antibiotic use, together with cautious collection of antibiotics and monitoring for resistance.
Stopping Recurrence, Greatest antibiotic for blended urogenital flora
Stopping recurrence of blended urogenital flora infections requires a complete method. This may occasionally contain sustaining good hygiene practices, avoiding sexual transmission, and finishing the complete course of antibiotics as directed by their healthcare supplier.
Sensitivity Testing and Cultures for Blended Urogenital Flora
Sensitivity testing and cultures are important elements within the prognosis and therapy of blended urogenital flora infections. These checks assist clinicians decide the best antibiotic remedy for a affected person by figuring out the particular micro organism inflicting the an infection and assessing the susceptibility of those micro organism to totally different antibiotics.
Strategies for Accumulating and Processing Specimens for Tradition and Sensitivity Testing
Specimens for tradition and sensitivity testing must be collected from the affected space utilizing sterile methods. This contains utilizing sterile gloves, swabs, and transport media to stop contamination and protect the integrity of the specimen. The kind of specimen collected will depend on the suspected web site of an infection, with urine, endocervical, and vaginal swabs being frequent sources. It’s important to think about the affected person’s signs, medical historical past, and danger elements for particular infections when deciding on the suitable specimen sort. As soon as collected, the specimen must be promptly transported to the laboratory for processing.
For urine specimens, the really helpful methodology is clean-catch midstream voiding, the place the affected person urinates a small quantity to scrub their genital space earlier than gathering a midstream void. This reduces the chance of contamination with regular vaginal flora.
Interpretation of Tradition and Sensitivity Outcomes
Tradition and sensitivity outcomes must be interpreted within the context of the affected person’s medical presentation and medical historical past. Constructive cultures point out the presence of a micro organism, whereas sensitivity testing outcomes present the extent of antimicrobial susceptibility. It’s important to think about each the kind of micro organism and the diploma of resistance when selecting an antibiotic.
Conditions in Which Tradition and Sensitivity Testing are Obligatory or Fascinating
Tradition and sensitivity testing are really helpful within the following conditions:
- Recurrent or persistent an infection: When a affected person experiences frequent or persistent infections, tradition and sensitivity testing can assist determine the underlying causes and information focused antibiotic remedy.
- Antibiotic failure: If a affected person exhibits no enchancment or experiences a relapse after finishing a course of antibiotics, tradition and sensitivity testing can assist determine resistant micro organism and information the collection of various antibiotics.
- Extreme an infection: In instances of extreme an infection, reminiscent of pelvic inflammatory illness or pyelonephritis, tradition and sensitivity testing is important to determine the causative micro organism and information immediate and efficient antibiotic remedy.
- Being pregnant or immunocompromised sufferers: In pregnant ladies or immunocompromised sufferers, correct identification of micro organism and evaluation of antibiotic resistance is essential to make sure efficient and secure therapy.
Complementary and Various Approaches for Blended Urogenital Flora
Complementary and various drugs approaches have gained consideration as potential remedies for blended urogenital flora infections. Whereas antibiotics stay the first therapy, some non-antibiotic therapies might provide various options. This part will discover the scientific proof supporting these approaches and share case research illustrating their effectiveness.
Natural Treatments
Natural cures have been used for hundreds of years to deal with numerous well being points, together with urogenital infections. Sure herbs, reminiscent of uva ursi, goldenseal, and barberry, possess antimicrobial properties that will assist fight blended urogenital flora. Uva ursi, specifically, has been proven to exhibit inhibition of bacterial progress, together with Escherichia coli, which is a typical reason behind blended urogenital infections. A research printed within the Journal of Various and Complementary Medication discovered {that a} uva ursi extract inhibited the expansion of E. coli by 70%.
- Uva ursi has been historically used to deal with urinary tract infections and could also be efficient in opposition to blended urogenital flora.
- Goldenseal and barberry additionally possess antimicrobial properties, though extra analysis is required to ascertain their efficacy in opposition to blended urogenital infections.
- Natural cures must be used with warning and beneath the steering of a healthcare skilled as a consequence of potential interactions with different medicines.
Probiotics
Probiotics are dwell microorganisms that confer well being advantages when administered in sufficient quantities. Probiotics might assist keep a wholesome steadiness of intestine flora, which might, in flip, forestall the overgrowth of micro organism related to blended urogenital infections. A research printed within the journal Vitamins discovered that probiotic supplementation elevated the degrees of Lactobacillus and Bifidobacterium within the vaginal flora, lowering the severity of blended urogenital infections.
“Probiotics could also be a helpful adjunct to plain antibiotic remedy for treating blended urogenital infections, notably in instances the place antibiotic resistance is a priority.”
- Probiotics containing Lactobacillus and Bifidobacterium strains could also be efficient in lowering the severity of blended urogenital infections.
- Probiotic dietary supplements must be chosen based mostly on the particular pressure and efficiency to make sure efficacy.
- Additional analysis is required to ascertain the optimum probiotic routine for blended urogenital infections.
Different Complementary Approaches
Different complementary approaches, reminiscent of acupuncture and homeopathy, have been steered as potential remedies for blended urogenital infections. Nevertheless, the scientific proof supporting these approaches is proscribed, and extra analysis is required to ascertain their efficacy. Moreover, some people might discover consolation in utilizing these approaches as a part of a holistic therapy plan.
- Acupuncture might assist alleviate signs reminiscent of ache and discomfort related to blended urogenital infections.
- Homeopathy has been steered as a therapy choice for blended urogenital infections, though extra analysis is required to ascertain its efficacy.
- Medical trials are important to ascertain the security and effectiveness of those approaches.
Closing Conclusion
We have mentioned the important antibiotics for treating blended urogenital flora infections, making an allowance for elements like patient-related issues, therapy regimens, and sensitivity testing. By understanding these facets, you’ll be able to navigate the therapy choices extra successfully and scale back the chance of long-term harm or problems.
Questions Typically Requested
What are the frequent causes of blended urogenital flora infections?
Blended urogenital flora infections are sometimes attributable to micro organism reminiscent of Escherichia coli, Klebsiella pneumoniae, and Enterobacter species.
Can blended urogenital flora infections be handled with over-the-counter antibiotics?
No, over-the-counter antibiotics is probably not efficient in treating blended urogenital flora infections, and their use can exacerbate the issue or promote antibiotic resistance.
What position does antibiotic resistance play in treating blended urogenital flora infections?
Antibiotic resistance is a big concern in treating blended urogenital flora infections, as resistant micro organism might develop and unfold, making therapy tougher.
Can life-style modifications assist forestall blended urogenital flora infections?
Sure, sustaining good hygiene practices, reminiscent of common bathing, handwashing, and avoiding sexual contact with contaminated companions, can assist forestall blended urogenital flora infections.